A number of recent articles about electronic medical records (EMRs) have argued that any new system should be tailored to the procedures in a hospital or the office of a doctor. The alternative is to build the system based on best practices and retrain the doctor and staff.
Looking at an EMR system for a single location will almost always lead to a tailored solution because it can be installed quicker and the cost and pain of installation appear to be lower. However, when an EMR system is looked at as part of a larger network—CCHIT: White Paper on interoperability—the pendulum swings to a best practice solution.
A useful analogy comes from early experience with word processing systems. Initially, each PC manufacturer provided a custom version of its own word processor. That worked as long as a PC was little more than an electronic typewriter that produced paper documents to be distributed. Documents prepared and printed in different offices where similar enough that the reader could ignore the variances. As offices began to share the electronic forms of documents between computers and with other offices (usually in the form of a floppy disk) tailored systems no longer worked. The word processing software became separate from the hardware and independent software firms like Microsoft, WordPerfect, and a few others became the standards, often within a particular industry. Microsoft Word eventually won, but now software from other companies like Google is showing up in response to changes in computer and network technology.
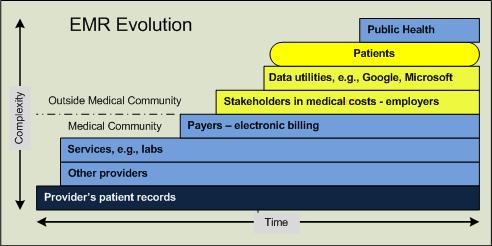
A unique EMR in a doctor’s office can function very well until the office sends or receives information from EMRs in the offices of other practitioners, laboratories, payers, public health, etc. Sooner or later the doctor’s system will have to be able to interface to other systems if it is to receive and provide the information needed by the doctor and her patients.
The selection and implementation of a best parctices EMR will require careful review of several systems to find the one that provides the features and functions required by a specific practice. Then options will have to be selected to tailor the system to that practice’s specific style.
The pros and cons of Tailored vs. Best Practices systems are listed in the following matrix. (Note: row numbers are provided for reference only; no ranking is intended except for the first row.)
|
# |
Tailored Solution |
Best Practice Solution |
|
1 |
Familiar, easier to implement which initially means lower cost and pain | New, requires retraining and breaking old habits, takes longer and costs more |
|
2 |
Built on a single practice, may or may not be best way or even a particularly good way | Takes advantage of experience of multiple practices to find best way or ways |
|
3 |
Uses experience with manual methods as a basis for an automated system, rather like using a bicycle as a model for a motorcycle | Based on a combination of manual and automated experience from multiple sources |
|
4 |
Current practices have to be documented before they can provide the basis for a new s6ystem, requires time and cost | Best practices have been defined and incorporated in new versions |
|
5 |
Each practice’s manual processes are imbedded in its systems | All locations using the same vendor/version have essentially the same processes, e.g., Microsoft Word is essentially the same in all offices |
|
6 |
A doctor who has a private and hospital(s) practice must learn a different system for each location | A doctor who has a private and hospital(s practice can move from one to the other in terms of using the system and the way information will be presented |
|
7 |
All training for the system will have to be tailored to the specific system | Standardized training material and classes can be used to train new employees and update current users |
|
8 |
Sysem training and best practice training such of some continuing education may conflict | System changes can be implemented to coincide with training in new and improved best practices as part of continuing education |
|
9 |
Networked users will have to become familiar with any unique features or functions of a doctor’s office increasing the risk of error and reducing the ease of use | Network users will find a standardized system easer to use which will in turn minimize the risk of errors. |
|
10 |
Each new member of the practice will have to be trained; this training will not improve their resume for future employment | Newly hired experienced users of standardized systems will get up to speed faster thus providing greater value to the office and will see improvements in their skills as career builders |
|
11 |
The substance and format of a question can shape the respondent’s answers. Differences in the questions or prompts on different systems can impact the answers in unforeseen ways. | Standardized questions in terms of both content and format reduce the variability of the answers of different respondents. Better initial answers increase the value of the subsequent use of the data. |
|
12 |
Changes in regulations or common practice require changes in each individual system; usually requires technical assistance | Changes in regulations or common practice can be made automatically for all comparable systems via automatic download – similar to version changes for common office software such as Word |
|
13 |
Each new computer application must be developed for a specific system | A new computer application can be developed for multiple systems and costs are shared over many system rather than just one. |
Posted for comment on Linkedin at: HealthCare Information Technology and at: Health Informatics Technology (HIT) View comments on these sites.